Corneal Transplant
Corneal Transplant

A corneal transplant, also called keratoplasty, is a surgical procedure to replace part of your cornea with corneal tissue from a donor. Your cornea is the transparent, dome-shaped surface of your eye that accounts for a large part of your eye’s focusing power. A cornea transplant can restore vision, reduce pain and improve the appearance of a damaged or diseased cornea. Most cornea transplant procedures are successful. But cornea transplant carries a small risk of complications, such as rejection of the donor cornea.
About 40,000 corneal transplants are performed in the U.S. every year.You may need a cornea transplant if your cornea no longer lets light enter your eye properly because of scarring or disease.
Why it is done?
A corneal transplant is most often used to restore vision to a person who has a damaged cornea. A cornea transplant may also relieve pain or other signs and symptoms associated with diseases of the cornea.
A number of conditions can be treated with a cornea transplant, including:
- A cornea that bulges outward (keratoconus)
- Fuchs’ dystrophy
- Thinning of the cornea
- Cornea scarring, caused by infection or injury
- Clouding of the cornea
- Swelling of the cornea
- Corneal ulcers, including those caused by infection
- Complications caused by previous eye surgery
Role of a Healthy Cornea
Your cornea is a clear tissue that covers the front of each eye. Light entering your eye first passes through the cornea, then your pupil (the dark spot at the center of the colored iris), and then your lens.The cornea must remain clear for you to see properly. However, a number of problems can damage the cornea, affecting your vision. These include:
- Corneal scarring from trauma and infection.
- Keratoconus, a degenerative condition in which the cornea becomes thin and misshapen.
- Inherited corneal conditions (dystrophies) like Fuchs’ dystrophy, Lattice dystrophy, and others.
Success Rates of Cornea Transplants
Experts know more about the long-term success rates of penetrating corneal transplants, which use all the layers of the cornea.
Success rates are also affected by the problem that needed to be fixed with the transplant. For example, research has found that the new cornea lasts for at least 10 years in:
- 89% of people with keratoconus
- 73% of people with Fuchs’ dystrophy
- 60% to 70% of people with corneal scarring
Corneal Donor
You don’t need to be worry about the corneal donation because we have a cornea bank which provides cornea to the needful patients.
Types of Cornea Transplants
The cornea contains five layers. Corneal transplants don’t always transfer all the layers.
Types of corneal transplants include:
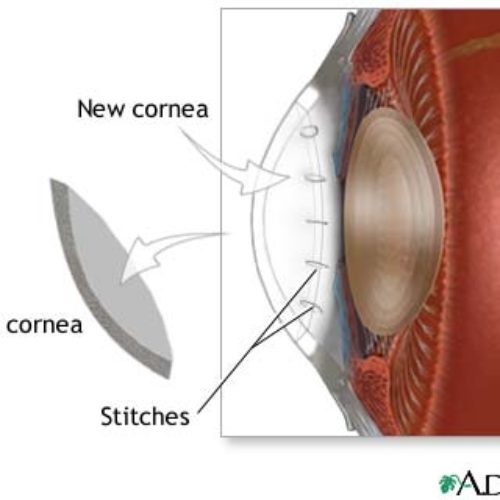
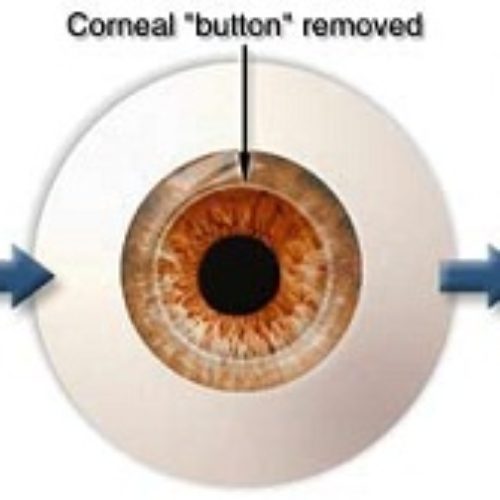
Penetrating (full thickness) cornea transplant
This involves transplanting all the layers of the cornea from the donor.
Lamellar cornea transplant
During this procedure, the surgeon only replaces some of the layers of the cornea with the transplant.
In a lamellar cornea transplant, selected layers are transplanted, which can include the deepest layer, called the endothelium (posterior lamellar cornea transplant). Commonly performed versions of this procedure include Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) or Descemet’s Membrane Endothelial Keratoplasty (DMEK).
Or it can include layers closer to the surface (anterior lamellar cornea transplant).
Lamellar transplants may be more appropriate than full penetrating transplants when the disease process is limited to only a portion of the cornea.
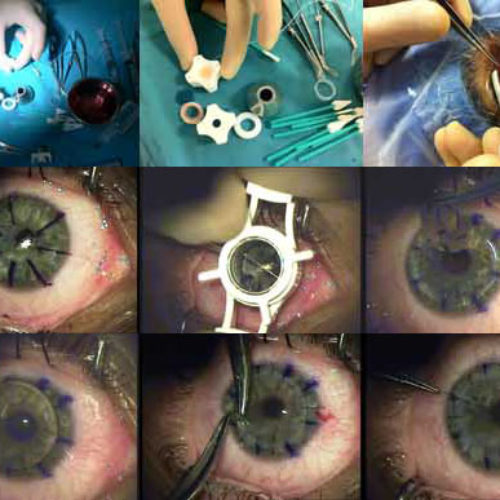
How Full Thickness Cornea Transplants Are Performed
The surgery can be done using local anesthesia. This uses medication to numb the eye and stop it from moving. The patient stays awake although sedated during the surgery.
Another option is general anesthesia. In this case, the patient is put to sleep for the procedure.
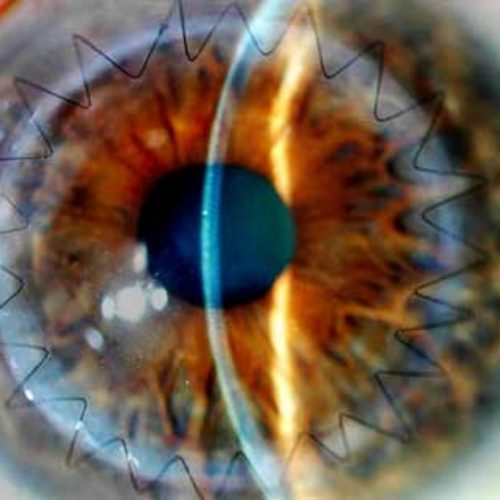
The surgeon uses a special cutting instrument called a trephine, which works like a cookie cutter. It removes a round section of damaged cornea from the front of your eye.
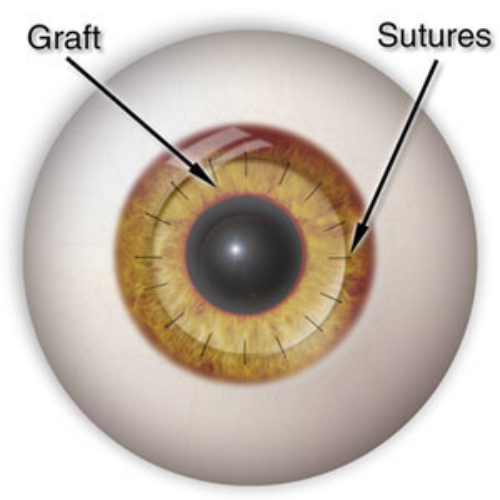
The same process is used to remove a similar-sized circle of cornea from the donor’s eye. The surgeon places the new section of cornea onto your eye. Then he or she sews it into place using ultra-thin stitches with the help of a microscope.
Recovery from a Corneal Transplant
The risks of complications vary depending on how many layers of the cornea are transplanted. The cornea is “immunologically privileged” so that no matching of donor to recipient is required. Additionally, steroid eye drops afford protection against rejection so that pills and systemic medications are not required to prevent rejection.Your body is even less likely to reject the transplant if only the outer layers are used, compared to using all the layers or the deepest layer. Rejection happens in less than 20% of cases overall.
Other problems can include:
- Bleeding (rare)
- Scarring
- Cataract formation, retinal detachment and damage to other parts of the eye
- Leakage of fluid from the transplant incision
- Infection (rare)
- Vision problems.
Full thickness transplants can heal with large amounts
of astigmatism, nearsightedness and farsightedness, requiring thick lenses on eyeglasses or contact lenses.
In addition, some ailments that damage people’s original cornea can also harm the new cornea. For example, there is the possibility of recurrence of herpes simplex infection in the transplant.
Persian International Health Tourism is a private company act as a facilitator between patients/visitors, best medical teams and various hospitals suggesting best available options based on your required treatment or other services.